Diabetic Eye Disease: Global Challenges to Diabetes Care
“The number of people with diabetes has nearly quadrupled since 1980 to 415 million adults today, and by 2040 is set to rise to 642 million, equating to roughly 10% of the global adult population aged between 20 and 79 years”
(International Diabetes Federation, 2015).
- Understanding eye disease as a complication of diabetes
- Difficulties in accessing and providing quality eye care
- Health system challenges
Understanding eye disease as a complication of diabetes
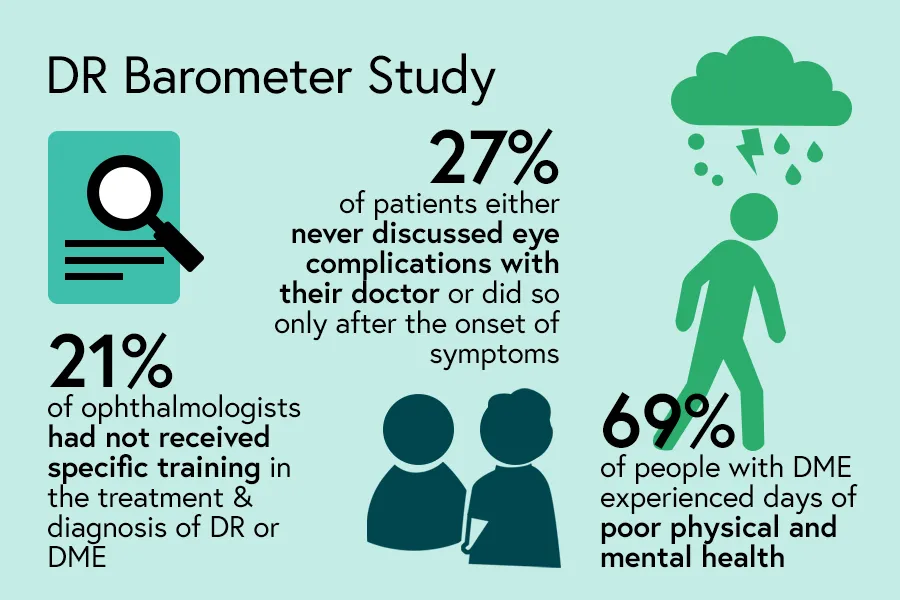
- Just under 40% of respondents who were people with diabetes reported being concerned about the risk of eye disease complications
- 27% either never discussed eye complications with their doctor or did so only after the onset of symptoms
“I can’t see properly, everything looks blurry, my eyes seem burning. I didn’t know that eye diseases were linked with diabetes.”
Person with diabetes, age 32, Bangladesh
“Yes, he told me frankly, that I should go and examine my eyes and meticulously follow up with the ophthalmologists. However, as I mentioned, I did not obey at the beginning. Sometimes, I would lie to him and say, “Yes, I did.” Only when I felt a problem I started following up meticulously.”
Person with diabetes, age 60, Saudi Arabia
“We are trying to draw their attention to the need of periodic ophthalmologic examinations. But unfortunately, we do not succeed 100% every time. A lot of our patients do not understand why they should come, even if they do not have anything with their eyes. “Why should I come?” they ask us. “Nothing upsets me,” they say.”
Ophthalmologist, Romania
- 79% said their vision impairment made everyday activities difficult, such as driving, working and cooking or cleaning their home, and in some cases impossible
- 69% of those with DME experienced days of poor physical and mental health
- 20% said their vision impairment made it difficult to manage their diabetes
“Sometimes…I am in a hall for a social occasion, and I get very shy because, I cannot really recognise a relative or friend’s face.”
Person with diabetes, age 60, Saudi Arabia
“My son has been very helpful. He is the one that also helps me buy things. If I get really bad, he takes me to the doctor. Right now, he’s asking me a lot of details about my diabetes. I guess the person that he’s talking to is asking him all of those things.”
Person with diabetes, age 50, Mexico
Difficulties in accessing and providing quality eye care
-
38% of patients said that long wait times for an appointment were a barrier to eye exams
-
21% of ophthalmologists had not received specific training in the treatment and diagnosis of DR or DME
“What I really miss is the real link between the doctors. Everyone is just interested in his own topic, and that’s it. Yes, they warn about other issues, but maybe once and that’s it. They never follow up.”
Person with diabetes, age 56, Saudi Arabia
“Patients … who need treatment require frequent clinic visits, but they are the working generation…, so they cannot take a day off for this. …they have difficulty in visiting clinic. And say laser treatment or anti-VEGF treatment for diabetic macular oedema cost quite a lot, and that makes patients hesitate to have treatment, …not all cases, but some,… so that can be a barrier to the services.”
Ophthalmologist, Japan
“[Patients] wait an irrational amount of time. There are patients who cannot get an appointment until four, five, six months later or more, in order to be seen when their condition must be treated as soon as possible. I think this is the main obstacle patients’ face – there are too many patients, and they can’t all be seen in a timely manner.”
Ophthalmologist, Mexico
Health system challenges
“Of the 20 ophthalmologists in Buenos Aires, there are only two places that can treat retinopathy.”
Diabetes educator, Argentina
“The equipment is expensive. This has always been the challenge. That has been one of the de-motivating issues. So [providers] know that if they train, some may not get the equipment.”
Ophthalmologist, Uganda
Table. Challenges for improving patient outcomes in diabetic eye disease
| Identified challenge | Percentage of ophthalmologists, % (n=563) |
|---|---|
| Late diagnosis | 66.3% |
| Limited access to patient education on DR and DME | 55.1% |
| Inadequate referral pathways | 41.7% |
| Multi-disciplinary team integration is poor | 39.1% |
| Reimbursement/restrictions on approved treatment | 35.7% |
| Government/insurance not able to cover patient costs | 31.3% |
| Ineffective screening services | 27.9% |
| No universal guidelines on referral/screening | 20.4% |
| No universal guidelines on how to treat | 13.9% |
| No universal guideline on when to treat | 12.1% |
| Current available therapies not effective | 6.9% |
| Other | 6.7% |
Strategic and specific investments are essential to ensure the necessary training for increased numbers of health care personnel and to develop cost effective and timely interventions. The goal should be to build sustainable business models for improved outcomes for diabetic eye diseases, as well as implementing national eye health policies and legislation to address the barriers to access and care.
The economic burden of diabetic retinopathy affects individuals, families and societies. For example, someone who can no longer work because of visual impairment from diabetic retinopathy requires family support, national welfare or disability funds and this drains resources.
An initial investment in a screening and treatment programme will prevent unnecessary health care dollars being spent further down the road on complications, surgery and advanced treatment for DR. In addition, the years of work people with diabetes gain from improved eyesight will directly benefit the economy and benefit the health care system on the whole. Research demonstrates that diabetes is among the top ten causes of death globally and – with the other three major non-communicable diseases (NCDs) of cardiovascular disease, cancer and respiratory disease – accounts for over 80% of all premature NCD deaths.
Effective multi-sectoral, interdisciplinary and co-ordinated responses using national and international public policies and timely interventions within and beyond the health sector, must be applied to overcome this devastating burden.
What do you think the key diabetes challenges are?
Which of the issues reported by the DR Barometer study stood out for you in your setting? What are the gaps that need to be addressed to strengthen the DR health system?
Written by Luxme Hariharan, Van Lansingh and Daksha Patel
Diabetic Eye Disease: Building Capacity To Prevent Blindness
Diabetic Eye Disease: Building Capacity To Prevent Blindness

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free







