Managing the Airways of COVID-19 Patients
The current global crisis caused by the Coronavirus Disease 2019 (COVID‐19) pandemic is causing enormous harm to the whole population: physically, psychologically, socially and financially. We stand in solidarity with all the people affected across the globe, and send our deepest sympathies to the families of those who are suffering the most during this time.
Airway management of the critically ill patient suffering from an infectious disease comes with its own particular challenges. Over the next few steps we will discuss personal protective equipment in the context of the modes of transmission of the virus, have a look at recently published airway management guidelines and share experiences, engaging in a global discussion. As evidence and recommendations are updated on a daily basis, we offer several links to external resources that are kept up-to date.
This article by Dr Maximilian Neun, Anaesthetic Speciality Registrar and Dr Damon Kamming, Consultant Anaesthetist at UCLH, summarises some key aspects of the epidemic, disease transmission and airway management.
At the end of 2019 a new coronavirus named SARS-CoV-2 and its associated disease, Coronavirus Disease 2019 (COVID-19) started spreading globally from the initial outbreak in Wuhan, China. On the 11th of March the WHO classified the outbreak as a global pandemic. As of the 12th of April 2020, over 1.6 million confirmed cases and over 100,000 deaths worldwide due to COVID-19 were registered[1].
Symptoms of infected individuals can vary widely from completely asymptomatic to Acute Respiratory Distress Syndrome (ARDS) with fulminant respiratory failure and multiorgan dysfunction. Around 5% of patients in China who tested positive for the virus required admission to intensive care [2]. Healthcare workers made up a significant proportion of infected patients with 3.8% of registered cases and 14.8% of infected healthcare staff suffered severe or critical disease [3]. Infection control and protection of healthcare staff have been huge challenges in the management of the pandemic.
The main mode of transmission of COVID-19 is via large respiratory droplets, as well as via direct contact (fomite) transfer of the virus. These virus-laden droplets have a diameter of more than 5-10 microns and usually disperse within a two-metre radius when emitted through sneezing and coughing by an infected patient. This is in contrast to airborne transmission, which differs from droplet transmission in the size of droplet nuclei, generally referring to particles smaller than 5 µmetres in diameter [4] These particles can remain in the air for a prolonged period of time, disperse further by following airflow and may penetrate standard surgical facemasks. A study of 75,465 COVID-19 cases in China did not report any cases of airborne transmission [5] and COVID-19 is currently not considered an airborne pathogen by the WHO or Public Health England, unless in the context of aerosol generating procedures (AGPs).
AGPs are medical interventions, such as tracheal intubation, non-invasive ventilation, tracheotomy, cardiopulmonary resuscitation, manual ventilation before intubation, and bronchoscopy, airway suctioning, nebulisation and high-flow nasal oxygen that can produce virus-laden aerosolised droplet nuclei of sizes small enough to be considered airborne [4].
Current UK guidelines therefore recommend that all health care staff performing aerosol generating procedures should wear personal protective equipment for airborne precautions, comprised of double gloves, a fluid resistant gown, eye or face protection and a filtering face piece (FFP) respirator [6], [7].
FFP2 respirators have to comply with the European standard EN 149: 2001 and have to block at least 95% of all particles of 0.3 microns in diameter or larger, whereas FFP3 respirators have to filter out at least 99%. Their American counterparts N95 and N99 respirators are certified by the National Institute for Occupational Safety and Health (NIOSH). All of the aforementioned respirators are capable of filtering out bacteria and viruses provided they form a good seal around the users mouth and nose.
During the SARS epidemic of 2003, health care workers were shown to be at a significantly increased risk of infection [8],[9] with tracheal intubation posing the highest risk procedure for transmission [10]. The correct use of personal protective equipment however, was able to reduce the incidence of transmission significantly [11], [12]. This includes the correct donning and doffing procedures for PPE, which should be performed with a trained observer acting as a ‘buddy’ following local guidelines to minimise healthcare worker coronavirus transmission [13].
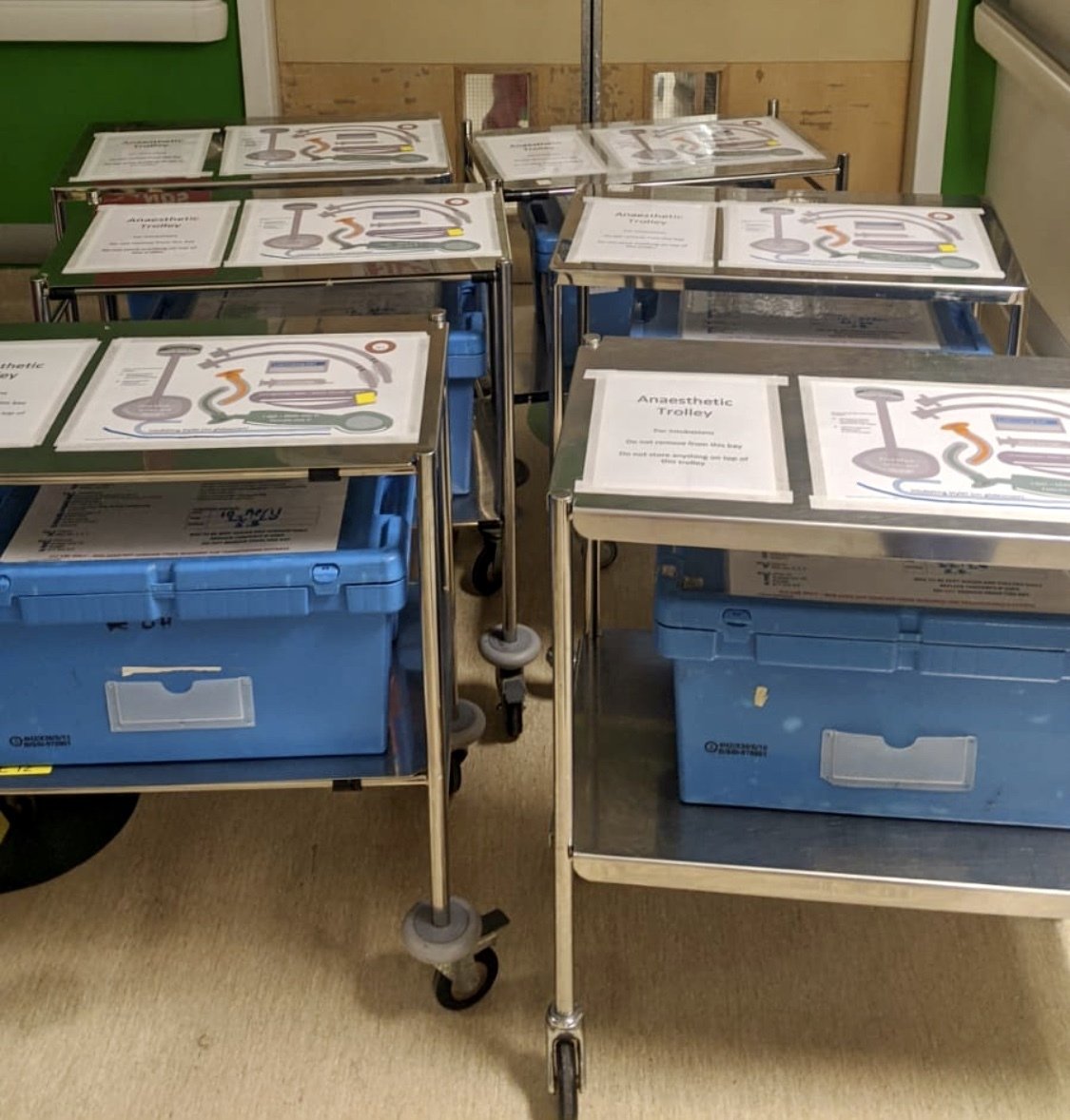 COVID-19 Airway trolleys and boxes
COVID-19 Airway trolleys and boxes
Emergency tracheal intubation in COVID-19 patients poses significant difficulties, owing to the degree of sickness of the patients and the added challenges of communication whilst working in full airborne precaution PPE. To ensure optimal team performance emergency intubation checklists need to be developed, dedicated COVID-19 equipment prepared (intubation mats, intubation boxes and dedicated intubation trolleys) and ideally the procedure rehearsed in a simulation setting [14]. Individual roles are allocated prior to entering a contaminated area. The most experienced anaesthetist should perform the intubation with the help of a videolaryngoscope to maximise the chance of a successful first intubation [7]. The ultimate aim is to ensure optimal patient and staff safety by performing airway management, adhering strictly to infection control recommendations, [13]
Currently, public healthcare interventions aim to control and prevent further spread of SARS-CoV-2. The risk of transmission by and to anaesthetists, intensivists and other healthcare workers can be minimised by correct usage of PPE and other interventions. Apart from PPE, how else can the spread of infection be prevented in the healthcare setting? In the next step Prof Tim Cook will discuss some key points.
References
8. Kamming D, Gardam M, Chung F. Anaesthesia and SARS. Br J Anaesth 2003
11. Nicole L. SARS safety and science. Can J Anesth 2003; 50: 983-8
Share this

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free








